
Before a treatment or rehabilitation protocol can be established, your physician must first determine the reason for, and source of, your condition. This typically involves a comprehensive physical examination and a detailed medical history profile, in addition to a complete history and description of the symptoms related to your condition. During this initial gathering of information, be sure to notify your doctor of any other illnesses, injuries, or complaints that have been associated with the pain or condition, as well as any previous treatments or medications prescribed. Preliminary diagnostic tests may then follow, including blood tests and/or X-rays.
Advanced Evaluation Procedures
Patients who require further evaluation may undergo one or more of the following:X-ray. A diagnostic test which uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film.
Arthrogram. An X-ray to view bone structures following an injection of a contrast fluid into a joint area. When the fluid leaks into an area that it does not belong, disease or injury may be considered, as a leak would provide evidence of a tear, opening, or blockage.
Magnetic resonance imaging (MRI). A diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body; can often determine damage or disease in a surrounding ligament or muscle.
Computed tomography scan (also called a CT or CAT scan). A diagnostic imaging procedure that uses a combination of X-rays and computer technology to produce horizontal, or axial, images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays
Electromyogram (EMG). A test to evaluate nerve and muscle function.
Ultrasound. A diagnostic technique which uses high-frequency sound waves to create an image of the internal organs Laboratory tests. Tests to determine if other problems may be the cause.
Arthroscopy. A minimally-invasive diagnostic and treatment procedure used for conditions of a joint. This procedure uses a small, lighted, optic tube (arthroscope) which is inserted into the joint through a small incision in the joint. Images of the inside of the joint are projected onto a screen; used to evaluate any degenerative and/or arthritic changes in the joint; to detect bone diseases and tumors; to determine the cause of bone pain and inflammation.
Myelogram. Involves the injection of a dye or contrast material into the spinal canal; a specific X-ray study that also allows careful evaluation of the spinal canal and nerve roots.
Radionuclide bone scan. A nuclear imaging technique that uses a very small amount of radioactive material, which is injected into the patient's bloodstream to be detected by a scanner. This test shows blood flow to the bone and cell activity within the bone.
After the evaluative information is collected and reviewed, the orthopaedist will discuss the treatment options with you, in order to help you select the best treatment plan that promotes an active and functional life.
PATIENT GUIDE: HIP REPLACEMENT
When Surgery Is Recommended
There are several reasons why your doctor may recommend hip replacement surgery. People who benefit from hip replacement surgery often have:
Candidates for Surgery
There are no absolute age or weight restrictions for total hip replacements
Total hip replacements have been performed successfully at all ages, from the young teenager with juvenile arthritis to the elderly patient with degenerative arthritis
Realistic Expectations
Most people who undergo hip replacement surgery experience a dramatic reduction of hip pain and a significant improvement in their ability to perform the common activities of daily living.
With normal use and activity, the material between the head and the socket of every hip replacement implant begins to wear. Excessive activity or being overweight may speed up this normal wear and cause the hip replacement to loosen and become painful. Therefore, most surgeons advise against high-impact activities such as running, jogging, jumping, or other high-impact sports.
Realistic activities following total hip replacement include unlimited walking, swimming, golf, driving, hiking, biking, dancing, and other low-impact sports.
With appropriate activity modification, hip replacements can last for many years.
Medical Evaluation
This is needed to make sure you are healthy enough to have the surgery and complete the recovery process. Many patients with chronic medical conditions, like heart disease, may also be evaluated by a specialist, such a cardiologist, before the surgery.
Tests
Several tests, such as blood and urine samples, an electrocardiogram (EKG), and chest x-rays, may be needed to help plan your surgery.
Preparing Your Skin
Your skin should not have any infections or irritations before surgery. If either is present, contact your orthopaedic surgeon for treatment to improve your skin before surgery.
Blood Donations
You may be advised to donate your own blood prior to surgery. It will be stored in the event you need blood after surgery.
Medications
Tell your orthopaedic surgeon about the medications you are taking. He or she or your primary care doctor will advise you which medications you should stop taking and which you can continue to take before surgery.
Dental Evaluation
Although infections after hip replacement are not common, an infection can occur if bacteria enter your bloodstream. Because bacteria can enter the bloodstream during dental procedures, major dental procedures (such as tooth extractions and periodontal work) should be completed before your hip replacement surgery. Routine cleaning of your teeth should be delayed for several weeks after surgery.
Urinary Evaluation
Individuals with a history of recent or frequent urinary infections should have a urological evaluation before surgery. Older men with prostate disease should consider completing required treatment before having surgery.
Social Planning
Although you will be able to walk with crutches or a walker soon after surgery, you will need some help for several weeks with such tasks as cooking, shopping, bathing, and laundry.
If you live alone a discharge planner at the hospital can help you make advance arrangements to have someone assist you at your home.
Home Planning
You will most likely be admitted to the hospital one day before surgery for medical evaluation
Anesthesia
After admission, you will be evaluated by a member of the anesthesia team. The most common types of anesthesia are spinal, epidural, or regional nerve block anesthesia (you are awake but your body is numb from the waist down) and general anaesthesia. The anesthesia team, with your input, will determine which type of anesthesia will be best for you.
Implant Components
Many different types of designs and materials are currently used in artificial hip joints. All of them consist of two basic components: the ball component (made of highly polished strong metal or ceramic material) and the socket component (a durable cup of plastic, ceramic or metal, which may have an outer metal shell).
The prosthetic components may be "press fit" into the bone to allow your bone to grow onto the components or they may be cemented into place. The decision to press fit or to cement the components is based on a number of factors, such as the quality and strength of your bone. A combination of a cemented stem and a non-cemented socket may also be used.
Your orthopaedic surgeon will choose the type of prosthesis that best meets your needs.

(Left) A standard cemented femoral component. (Center) A standard un-cemented femoral component (Right) A small uncemented femoral component

(Top) The acetabular component shows the ceramic liner inside the metal shell. (Middle) Metal liner inside the metal shell(Bottom) Polyethylene liner inside the metal shell
Procedure
The surgical procedure takes a few hours. Your orthopaedic surgeon will remove the damaged cartilage and bone and then position new metal, plastic, or ceramic implants to restore the alignment and function of your hip.

X-rays before and after total hip replacement. In this case, non-cemented components were used.
After surgery, you will be moved to the recovery room where you will remain for several hours while your recovery from anesthesia is monitored. After you wake up, you will be taken to your hospital room.
You will most likely stay in the hospital for a few days. To protect your hip during early recovery, a positioning splint, such as a foam pillow placed between your legs, may be used.
Pain Management
After surgery, you will feel some pain, but your surgeon and nurses will provide medication to make you feel as comfortable as possible. Pain management is an important part of your recovery. Movement will begin soon after surgery, and when you feel less pain, you can start moving sooner and get your strength back more quickly. Talk with your surgeon if postoperative pain becomes a problem.
Physical Therapy
Walking and light activity are important to your recovery and will begin the day of or the day after your surgery. Most patients who undergo total hip replacement begin standing and walking with the help of a walking support the day after surgery. The physical therapist will teach you specific exercises to strengthen your hip and restore movement for walking and other normal daily activities.
Preventing Pneumonia
It is common for patients to have shallow breathing in the early postoperative period. This is usually due to the effects of anesthesia, pain medications, and increased time spent in bed. This shallow breathing can lead to a partial collapse of the lungs (termed "atelectasis") which can make patients susceptible to pneumonia. To help prevent this, it is important to take frequent deep breaths. Your nurse may provide a simple breathing apparatus called a spirometer to encourage you to take deep breaths.
The success of your surgery will depend in large measure on how well you follow your orthopaedic surgeon's instructions regarding home care during the first few weeks after surgery.
Wound Care
You may have stitches or staples running along your wound or a suture beneath your skin. The stitches or staples will be removed approximately 2 weeks after surgery.
Avoid getting the wound wet until it has thoroughly sealed and dried. You may continue to bandage the wound to prevent irritation from clothing or support stockings.
Diet
Some loss of appetite is common for several weeks after surgery. A balanced diet, often with an iron supplement, is important to promote proper tissue healing and restore muscle strength. Be sure to drink plenty of fluids.
Activity
Exercise is a critical component of home care, particularly during the first few weeks after surgery. You should be able to resume most normal light activities of daily living within 3 to 6 weeks following surgery. Some discomfort with activity and at night is common for several weeks.
Your activity program should include :
The complication rate following hip replacement surgery is low. Serious complications, such as joint infection, occur in less than 2% of patients. Major medical complications, such as heart attack or stroke, occur even less frequently. However, chronic illnesses may increase the potential for complications. Although uncommon, when these complications occur they can prolong or limit full recovery.
Infection
Infection may occur superficially in the wound or deep around the prosthesis. It may happen while in the hospital or after you go home. It may even occur years later.
Minor infections of the wound are generally treated with antibiotics. Major or deep infections may require more surgery and removal of the prosthesis. Any infection in your body can spread to your joint replacement.
Blood Clots

Blood clots may form in the leg veins or pelvis.
Blood clots in the leg veins or pelvis are the most common complication of hip replacement surgery. These clots can be life-threatening if they break free and travel to your lungs. Your orthopaedic surgeon will outline a prevention program which may include blood thinning medications, support hose, inflatable leg coverings, ankle pump exercises, and early mobilization.Leg-length Inequality
Sometimes after a hip replacement, one leg may feel longer or shorter than the other. Your orthopaedic surgeon will make every effort to make your leg lengths even, but may lengthen or shorten your leg slightly in order to maximize the stability and biomechanics of the hip. Some patients may feel more comfortable with a shoe lift after surgery.
Dislocation
This occurs when the ball comes out of the socket. The risk for dislocation is greatest in the first few months after surgery while the tissues are healing. Dislocation is uncommon. If the ball does come out of the socket, a closed reduction usually can put it back into place without the need for more surgery. In situations in which the hip continues to dislocate, further surgery may be necessary.

Hip implant dislocation
Loosening and Implant Wear Over years, the hip prosthesis may wear out or loosen. This is most often due to everyday activity. It can also result from a biologic thinning of the bone called osteolysis. If loosening is painful, a second surgery called a revision may be necessary.Other Complications
Nerve and blood vessel injury, bleeding, fracture, and stiffness can occur. In a small number of patients, some pain can continue or new pain can occur after surgery.
Recognizing the Signs of a Blood Clot
Follow your orthopaedic surgeon's instructions carefully to reduce the risk of blood clots developing during the first several weeks of your recovery. He or she may recommend that you continue taking the blood thinning medication you started in the hospital. Notify your doctor immediately if you develop any of the following warning signs.
Warning signs of blood clots. The warning signs of possible blood clot in your leg include :
Warning signs of pulmonary embolism. The warning signs that a blood clot has traveled to your lung include:
Preventing Infection
A common cause of infection following hip replacement surgery is from bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections.
Following your surgery, you may need to take antibiotics prior to dental work, including dental cleanings, or any surgical procedure that could allow bacteria to enter your bloodstream.
Warning signs of infection. Notify your doctor immediately if you develop any of the following signs of a possible hip replacement infection:
A fall during the first few weeks after surgery can damage your new hip and may result in a need for more surgery. Stairs are a particular hazard until your hip is strong and mobile. You should use a cane, crutches, a walker, or handrails or have someone help you until you improve your balance, flexibility, and strength.
Your orthopaedic surgeon and physical therapist will help you decide which assistive aides will be required following surgery, and when those aides can safely be discontinued.
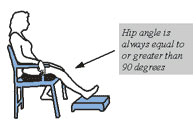
Below is a general list of precautions to follow after your total hip replacement. If additional precautions are necessary, the staff will provide instructions.
Lying Down


Your surgeon or therapist will tell you when to start sitting in a high chair.
Do:
Don't:
If you leave the hospital by car, to avoid bending your hip too far; sit in the front seat, making sure the car seat is all the way back and in an upright position. Sit on two pillows.

 Call us: +91884-2388888, 6668888
Call us: +91884-2388888, 6668888



